Swiftaid Update
April 24, 20242024 Year in Review – part 2
March 7, 2025Mauris rhoncus orci in imperdiet placerat.
Vestibulum euismod nisl suscipit ligula volutpat, a feugiat urna maximus. Cras massa nibh, tincidunt ut eros a, vulputate consequat odio.
Vestibulum vehicula tempor nulla, sed hendrerit urna interdum in. Donec et nibh maximus, congue est eu, mattis nunc. Praesent ut quam quis quam venenatis fringilla. Morbi vestibulum id tellus commodo mattis. Aliquam erat volutpat. Aenean accumsan id mi nec semper.

2024 mission stats
Number of call-outs
Call-outs by critical care car
Call-outs by helicopter
The areas we were called to

We were called out 15 times on our busiest day (Monday 22 July)
For the first time we surpassed 200 call-outs in a month (March, May, July)
Each mission costs £2,200 on average
Each day we were called to over six people on average
patients were given a pre-hospital emergency anaesthetic
patients were given emergency blood transfusions
I can’t thank the whole team enough for how they helped Lily. We are honoured to have these lovely people to attend trauma and life-threatening situations.

Lily's story
When Lily fell off her pony, she was dragged around the arena twice before her pony went over a jump which released Lily’s foot from the stirrup. With a broken femur and in severe pain, Critical Care Doctor, Chris Arrowsmith and Specialist Paramedic in Critical Care, Matt Robinson, jumped into the helicopter, reaching her in ten minutes. They pulled her leg back into place, administered pain killers and kept Lily comfortable and at ease while they travelled with her to hospital.
WE ENHANCED THE SKILLS OF OTHERS TO SAVE MORE LIVES
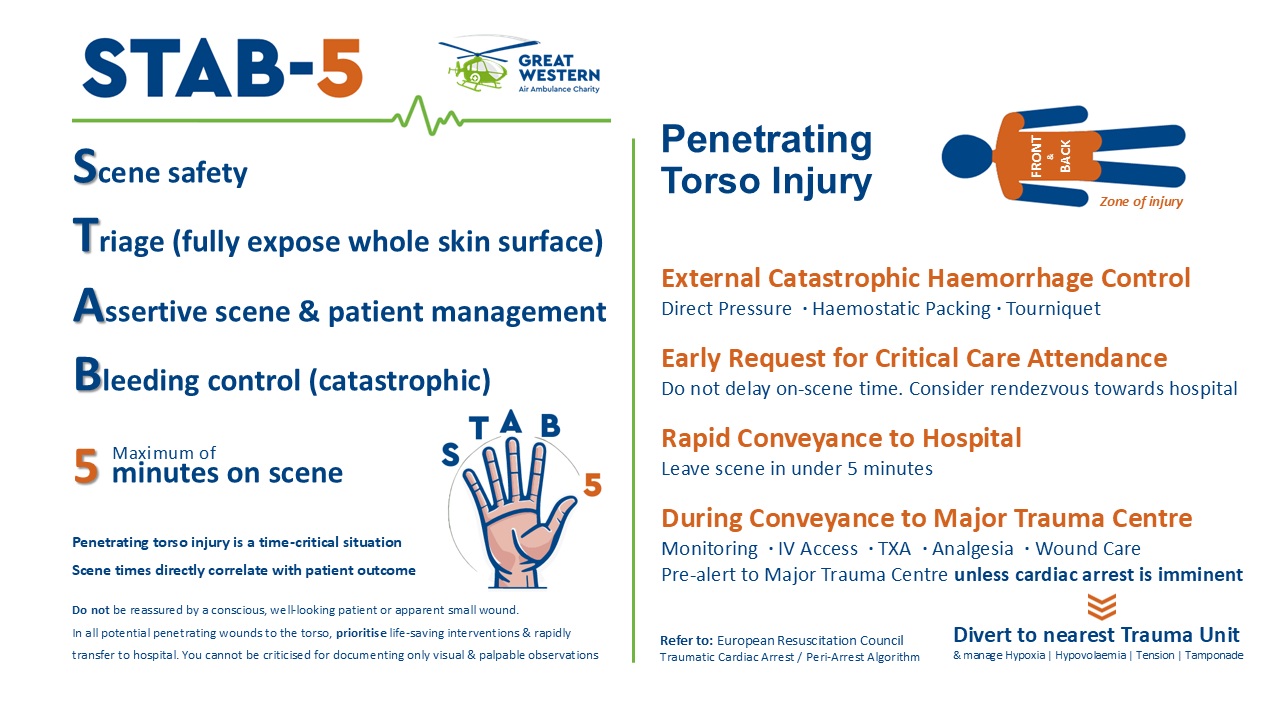
The STAB-5 mnemonic was created to help paramedics prioritise getting the patient on their way to hospital within five minutes of arrival on scene. By delaying routine observations or performing them en route the patient can receive critical care quicker to improve their chances of survival.
STAB-5 was adopted by the Welsh Ambulance Service, South Central Ambulance Service and Avon and Somerset Police. It was also translated into French, Spanish, Italian and Norwegian and published in the International Critical Care Journal.
This not only harnessed their clinical wisdom and experience into something that can make a real difference to patient care but shows how our outreach work is leading to further positive clinical innovations.
We started to trial a new patient pathway for cardiac arrest patients
In collaboration with the Bristol Heart Institute, we piloted an innovative pathway for patients in cardiac arrest and shockable rhythms, where defibrillation hasn’t worked. The patient continues to receive critical care and resuscitation en route to access specialist intervention, while still in cardiac arrest, with the potential to survive. This could offer a complex and exciting clinical pathway to help more people survive a cardiac arrest.

We collaborated on a pilot project to increase the provision of PHEA
In March, we embarked on a UK first pilot project with South Western Ambulance Service NHS Foundation Trust to assess the feasibility of an Advanced Clinical Practitioner in Critical Care delivering Pre-Hospital Emergency Anaesthesia (PHEA) to select adult patients. The goal is to improve the availability of time critical lifesaving care to patients in need with the hope that it can lead to positive changes in UK pre-hospital care, aligning with practice in many other countries.

WE WELCOMED SIX NEW CREW MEMBERS
One Pre-Hospital Emergency Medicine (PHEM) trainee
Dr Celestrine Weegenaar
Celestine started with us in August as our newest PHEM Trainee. Originally from Amsterdam, she moved to Bristol in 2009 for medical school and has worked in a range of hospitals across our region. Dr Celestine’s goal is to qualify as a Critical Care Doctor at GWAAC and achieve a consultant role at either the BRI or Southmead Hospital.
I already knew some consultants who worked at GWAAC from my hospital work in the region and I heard so many good things about it. I decided I wanted to be the first female trainee at GWAAC.
Two Trainee Specialist Paramedics in Critical Care
James Leavor
James worked as a Paramedic in Exeter’s Hazardous Area Response Team Before joining us in June. He completed an enhanced clinical skills courseband instructed at the National Resilience Response Unit.
“I feel very lucky to have been selected to be a part of this ambitious and determined team.”
Waldo Zweep
Waldo was an Emergency Care Practitioner in South Africa’s HEMS (helicopter emergency medical service) and Retrieval before he moved to the UK in March 2023. He worked with South East Coast Ambulance Service until he joined us in June 2024.
“It’s very different to the system in South Africa but everyone has been very supportive.”
Three Critical Care Doctors
All three doctors joined us from other air ambulance charities, demonstrating the excellent reputation that GWAAC has for clinical care.

WE REDUCED INEQUALITIES IN PRE-HOSPITAL EMERGENCY MEDICINE TRAINING
Dr. Nicky Moore, along with PHEM trainees Dr. Mark Winstanley and Dr. Celestine Weegenaar, led the Access to PHEM (pre-hospital emergency medicine) programme for junior trainees in the Severn Deanery (a postgraduate medical education region in southwest England) aiming to improve access and support for local applicants to PHEM.
The initiative focused on offering education, mentorship and interview preparation to address barriers to transitioning from hospital practice to pre-hospital care, especially for underrepresented groups such as female doctors.
The programme included four introduction to PHEM sessions with talks from experienced clinicians, a base tour, and a Q&A. Participants received offers of pre-hospital experiences, contacts and ongoing informal mentorship from a group of local doctors who had recently been through PHEM training.

We hosted our second Fem in PHEM event
In August Specialist Paramedic, Fleur Rath, hosted our second Fem in PHEM event, bringing together over 50 female clinicians at the airbase and online. The event supported women in healthcare by providing guidance on entering the competitive field of Pre- Hospital Emergency Medicine (PHEM) and addressing the barriers that contribute to their underrepresentation.
Six speakers, including female members of our Critical Care Team and guest experts, shared insights on critical care, building a strong CV, career journeys in PHEM, confidence and imposter syndrome, and training pathways for paramedics and doctors. A panel Q&A provided attendees the opportunity to engage directly with experts in the field.
The event welcomed doctors, paramedics, and nurses from diverse backgrounds, all eager to explore opportunities for women in PHEM.
WE REDUCED OUR IMPACE ON THE ENVIRONMENT
We installed rooftop solar panels
We installed 560 solar panels on our airbase roof to help cut energy costs and CO2 emissions. Generating over 200,000 kWh annually – enough for 63 homes – the system feeds into the local grid and will save nearly 240 tonnes of CO2 over its lifetime.
Our thanks go to Bristol Energy Cooperative who funded most of the solar panels and now manage the installation, Beacon Owl Trust for additional funding and County Air Ambulance HELP Appeal for funding the necessary electrical upgrade.
This 240kWp solar PV system will supply affordable, sustainable energy for 25+ years, reducing our annual energy bills by £7,500. These savings allow us to help more people in urgent need of lifesaving care.

We improved our recycling and re-use efforts by opening two new shops



In addition to generating vital funds through the sale of 232,498 items and raising awareness through a stronger presence in local communities, our shops diverted thousands of tonnes of items from landfills, giving them a second life.
Bath, April
Situated on Moorland Road, we opened the first air ambulance charity shop in Bath. The eighth shop in our portfolio, it has given us a great opportunity to enhance our visual presence in the city offering its residents and visitors a unique opportunity to support GWAAC – if local people are in need of expert critical care, it is GWAAC that will be called.
Keynsham, June
Located in the bustling heart of Keynsham, our ninth shop became our second in the Bath & North East Somerset area. Its opening strengthens our presence in this region, connecting even more supporters to our vital work.

WE WORKED WITH COMMUNITIES TO STRENGTHEN THE CHAIN OF SURVIVAL
We helped communities install 66 new defibs, including placing more public access defibrillators in priority locations
Our Great Western Hearts defibrillator package makes it easy for anyone to raise funds and install a defib in their local community, to help save lives. Our project raised £213,806 in 2024 and we ended the year with 137 public access defibrillators in place across our region.
- 46 defibrillators in our network were used 150 times last year
- Three defibs were purchased for our charity pool cars
- Primary guardian volunteers checked 99 community defibs monthly

In 2024 Great Western Hearts taught 9,684 people:
people were taught CPR and defibrillation:
school students
people at community events
members of staff in businesses
students were taught first aid for a stabbing injury
93 volunteers gave 1,267 hours to teach in our communities,
including in 31 schools
across our region
If it weren’t for your quick timing, knowledge and perseverance, Nonna would have either died or had severe brain damage.